
Plantar fasciitis – what causes it and how to manage it?
Plantar fasciitis, plantar fasciopathy, policeman’s heel… whatever you want to call it, it essentially means that if you have this, you will be suffering with pain under your heel or in the arch of your foot. Plantar fasciitis is the most common cause for pain under your heel. Up to 7% of the general population will be suffering with this condition.
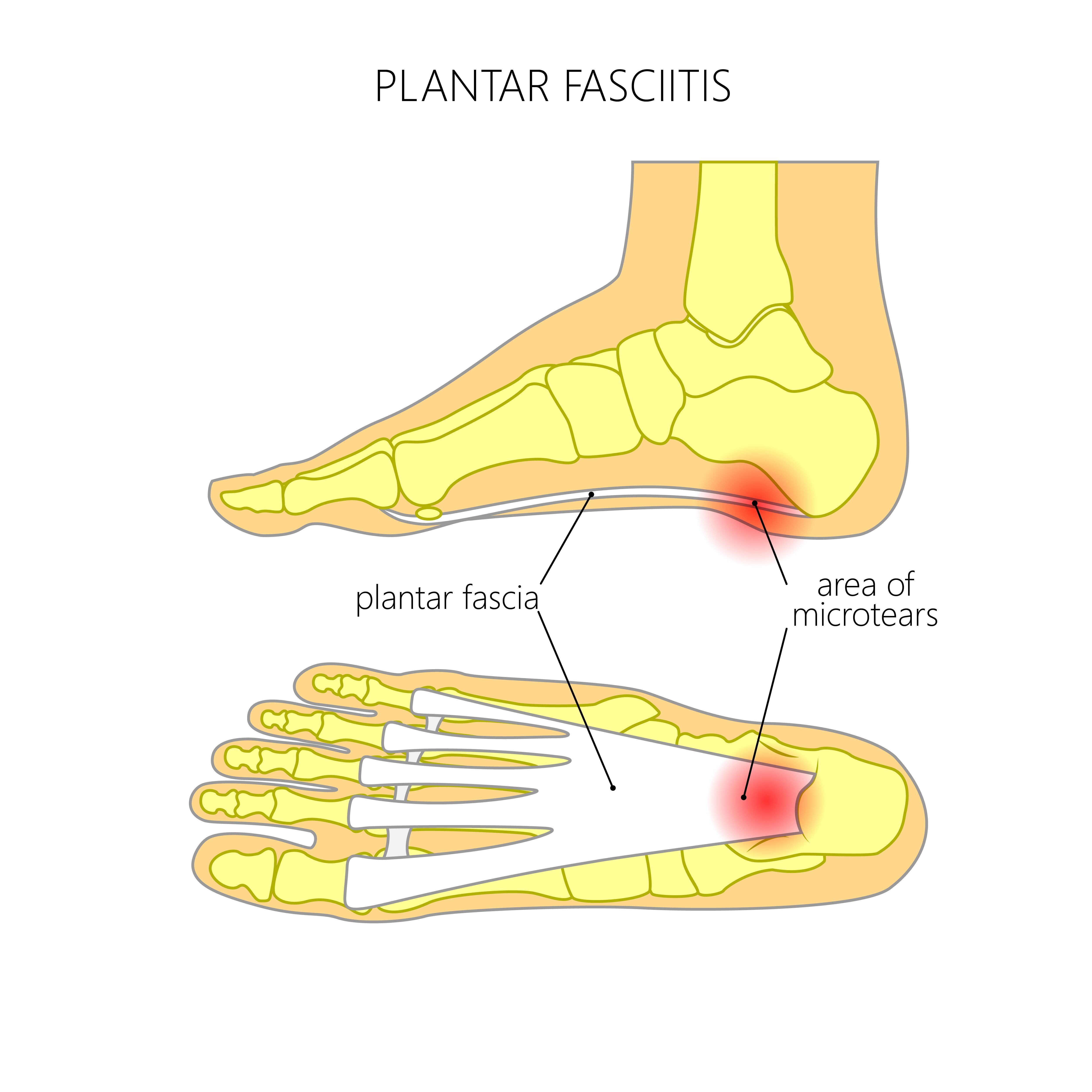
The plantar fascia is a thick connective tissue, which supports the arch on the plantar side of the foot (the bottom), and therefore plays an important role in weight bearing within the gait cycle. It runs from the tuberosity of the calcaneus (heel bone) and fans out towards the metatarsals (toes).
So what is plantarfasciitis? Despite the suffix – ‘itis’ – there is actually little to no inflammation, in fact it tends to be more of a degeneration of the fascia, or more commonly understood as an overuse injury. It will often feel like a burning pain under your heel or arch of your foot, which is typically worse after a period of inactivity. This is most noticeable in the morning, after you have been still all night whilst in bed. Some patients report that the pain makes it feel like they are standing on a pebble or stone too. Usually the pain eases after taking a few steps.
There are various risk factors, which may make you more at risk of developing plantar fascia pain. These can include:
- Foot biomechanics – including pes planus or pes cavus (flat feet or high arches) – as this changes the load absorbed by the plantar fascia in weight bearing and during the gait cycle
- Being overweight – as of course this generally increases the load through the fascia
- Inappropriate training – so increasing your running distance for example, as it previously said it can be from overuse
- Sports/exercise such as running (particularly long distance and road runners), dancers (especially ballet), and any sports involving lots of explosive jumping
- Standing on your feet all day
- Generalised weakness or deconditioning of the ankle/lower limb muscles
- Reduced range of movement at the ankle
So as you can see, the list is extensive! And I am sure there are some I have missed… therefore, when being seen by a physiotherapist for this; expect a thorough assessment. It also makes sense that plantar fasciitis is therefore treated holistically, as the onset is often not due to one definitive thing.
How To Improve your symptoms?
Now – to the important bit! What can you do to improve your symptoms? First of all, it is important to offload the fascia, which in turn should help to settle your symptoms. This means you may need to reduce your activity levels for a short time. I often say to my patients that if their pain is reaching levels of over 5 out of 10, then they are overdoing it. Similarly, if their pain flares up for several hours or even days following exercise, then they are definitely doing too much. During this initial phase, I recommend the use of pain relief as required, and ice massage. This can be done by freezing a bottle of water and then rolling it under the arch of the foot. I am happy for patients to use tennis balls to roll on the bottom of their feet if this helps too.
Once we have settled your symptoms down a little, its then important to begin gradual, graded exercise. The fascia will typically respond well to being loaded, and will adapt as necessary, as long as we take our time and don’t overdo it. Research has identified that high load strength training can be effective for plantar fasciitis. It is by no means a miracle cure, but has shown promising outcomes, and I find that one simple exercise, with progressions, is enough to improve symptoms with the patients I see in clinic.
The exercise recommended, both within the literature and from my professional experience, is a simple heel raise. To start with, this can be done with both feet on the floor. To progress, use a rolled up towel to extend the toe upwardly and applying a further stretch/load to the fascia. This can further be progressed by doing it one just one leg, and finally to doing it over the edge of a step. The most crucial part of this exercise is that it must be done slow and controlled; I often operate a rule of three (3s up, 3s hold, 3s lower). A good starting place is three sets of 10. From here, you can judge whether it is easy and you need to progress, which can be doing either by increasing repetitions, or progressing the exercise as already mentioned.
References:
Badatunde, O. O., Legha, A., Littlewood, C., Chesterton, L. S., Thomas, M. J., Menz, H. B., Van der Windt, D., Roddy, E., 2018. Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. British Journal of Sports Medicine (online).
Hill, C. L., Gill, T. K., Menz, H. B., Taylor, A. W., 2008. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. Journal of Foot and Ankle Research (online). 1 (1)
Rathleff, M. S., Molgaard, C. M., Fredberg, U., et al. 2014. High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up. Scandinavian Journal of Medicine and Science in Sport (online).
Santiago, R. O., Leon, M. R., De las Penas, C. F., Manzano, G. P., Moreno, J. S., 2018. Ultrasound imaging and health related to quality of life in patients with chronic plantar heel pain. Rehabilitative Ultrasound Imaging (online).



No Comments yet!